Johns Hopkins Daily Covid Map
First Response
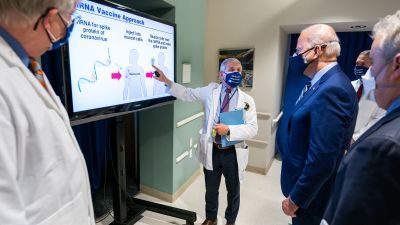
Early on December 9, a 90-year-old British woman named Margaret Keenan became the first to receive a COVID-19 vaccine in the Western world who wasn’t part of a clinical trial. (In a delightful quirk of the English language, the BBC writeup called receiving the vaccine “getting the jab.”) There’s every expectation that the Pfizer vaccine will be approved for use in the U.S. in a matter of days, and should begin to roll out among the first hospital workers and nursing home residents by the weekend. There’s even evidence, issued by the FDA this morning, that the vaccine is effective after the first dose of the two-dose sequence.
It’s a big moment for science, but it will be mediated through the block and tackle of logistics. There will be plenty of second-guessing throughout the next six months on the right and wrong way to deploy the vaccines, so it’s worth looking at what’s a valid criticism and what isn’t.
This thing that bubbled up yesterday about the U.S. having the opportunity to secure more doses of the Pfizer vaccine over the summer but declining falls into the “not that significant” category (h/t Kevin Drum). At the time, the race for a vaccine was on, and the government, not knowing which vaccine would actually be ready, spread itself across enough purchases to cover 150 percent of the entire U.S. population, with five different companies. That way, even if the trials fizzled, there would still be enough for everyone necessary to vaccinate.
Pfizer was one of these five, with enough pre-purchased for 50 million people. Moderna and AstraZeneca, which have both shown enough results in Stage 3 trials to raise expectations that they will be approved as well, add doses for another 200 million. So there are 250 million in the queue already, for a country of 330 million. If Johnson & Johnson or Novavax come through then there will be more than enough available. It made sense to get some doses with a lot of different manufacturers.
The main problem on the vaccine will involve literally not having enough raw materials to produce it. This has already been a challenge for Pfizer, leading to reductions in output in the early stages. The company wouldn’t say what they were missing, though there are a lot of discrete sources that go into the vaccine; antiseptic liquids, DNA of the virus, sterile water, etc. That doesn’t include the ultra-cold freezers (or in some cases, dry ice) you need to store the vaccine, the glass vials you need to hold it, the syringes and needles you need to, well, jab it, and so on. It’s the largest supply chain in history, and though this time companies had months of advance warning, the scale is unprecedented.
There have been periodic shortages of the carbon dioxide needed to create dry ice. (Check the atmosphere!) There are contingencies for glass vials and syringes, but of course then you have to wonder about the normal, everyday needs in the health system for these products. There are bound to be some supply chain issues.
Perhaps the greatest logistical fear is more of a political economy problem, where poorer nations simply cannot acquire the vaccine. This is as stupid as denying health care to the undocumented, when they’re our neighbors and house cleaners and food preparers; this will make us sicker and more prone to outbreaks (and potential mutations, at which point the vaccine could become less effective). But given that demand for vaccines will outstrip the supply, richer countries will simply have more ability to “stampede” their poorer counterparts.
Top UN officials are warning of a “humanitarian catastrophe” if the developing world cannot access the vaccine. There’s a simple solution to this, embedded in a call to share the intellectual property on the compound. “A lion’s share of the limited number of first doses have already been snatched up by a handful of countries… leaving very little for other countries in the short term,” said Dr. Sidney Wong, Executive Co-Director of Médecins Sans Frontières’ Access Campaign, in a statement. “What we really want to see is a rapid expansion of the overall global supply, so there are more vaccines to go around and doses can be allocated according to WHO’s public health criteria, not a country’s ability to pay.”
There’s some good news on this front. Moderna has said it would not enforce its patent on the vaccine, but hasn’t said it would share the IP. Pfizer has offered even less of a commitment. There’s been no promise to sell the vaccine at cost, and the proposed prices have been high. The U.S. and other nations paid for the R&D, and therefore could manufacture the drug itself to secure the required supply. Instead the companies have been allowed to set their own prices.
This is going to be a gut-check moment for the world’s richest nations and in some sense they’re already failing. Economic sanctions on countries like Iran are already impeding access to the vaccine. Covax, the WHO entity designed to get the vaccine out equitably, hasn’t been able to take payments from Iran. This is completely self-destructive and will prolong the crisis, for the sake of pharmaceutical profit. The supply chain we have to worry about is the one that gets help to the developing world.
Days Without a Bailout Oversight Chair
256.
Today I Learned
- Josh Hawley and Bernie Sanders may team up to add stimulus checks into the relief package. (Washington Post)
- Meanwhile, it’s the same problem as ever: Mitch McConnell is dug in on an extreme version of corporate legal immunity. (Politico)
- One estimate finds that the economy needs between $3 and $4.5 trillion to cover the demand shortfall. Any relief package at most covers a third of that. (Groundwork Collaborative)
- Soot in the atmosphere correlates with COVID deaths. The EPA could tighten the soot rule to reduce the impact. It’s choosing not to. (New York Times)
- A top index for commercial real estate is foundering. (Calculated Risk)
- The crisis has actually spurred interest in medical school. (NPR)
- Florida law enforcement agents raid the home of a woman conducting her own dashboard of COVID cases in the state. (Tallahassee Democrat)
- A list of all NYC businesses closed during the pandemic. (Curbed NYC)