Nurse Barbara Smith, left, and Dr. Bryan Christensen demonstrate the proper way for health care workers to use personal protective equipment when dealing with Ebola during an education session in New York, Tuesday, Oct. 21, 2014. (AP Photo/Seth Wenig)
While the disease is ravaging Sierra Leone, Liberia and Guinea, the reality is that Ebola is just not a serious First World problem. As devastating as the disease is, it’s not easily spread, and that makes it a poor candidate for a catastrophic outbreak in countries with functional health care systems (On Monday, the World Health Organization declared Nigeria’s outbreak at an end after the country had gone six weeks without a new case. Senegal got the all-clear a week earlier).
Terry O’Sullivan, a political scientist at the University of Akron who studies catastrophic infectious disease outbreaks — and health care systems’ capacity to cope with them — told BillMoyers.com that the Ebola scare is “a shot across the bow.”
“This is not the big one. Ebola will be contained. We might get a handful of cases — maybe even a few dozen, at most, by next year. But this is not something that’s going to race through the population,” he says.
O’Sullivan says the most important thing to understand in terms of our ability to cope with such a real pandemic scenario is that “we have been starving public health for the last 10 years despite the 9/11 attacks and the anthrax attacks.” The US has cut funding not only for the National Institutes for Health and the Centers for Disease Control, but also slashed its contribution to the World Health Organization. And USA Today reports that since 2008, “state and local health departments have cut more than 50,000 staff positions — about 20% of their workforce.”
“This is a classic situation where the lack of a fire has led people to shortchange the fire department,” says O’Sullivan.
But the problem goes beyond the budgets of a few public health agencies. The very structure of our health care system leaves us unprepared for a major catastrophe. Among the developed countries in the Organization for Economic Cooperation and Development (OECD), only Mexico relies more heavily than the United States on the private sector to provide health care, but a robust public health system is best equipped to deal with an epidemic.
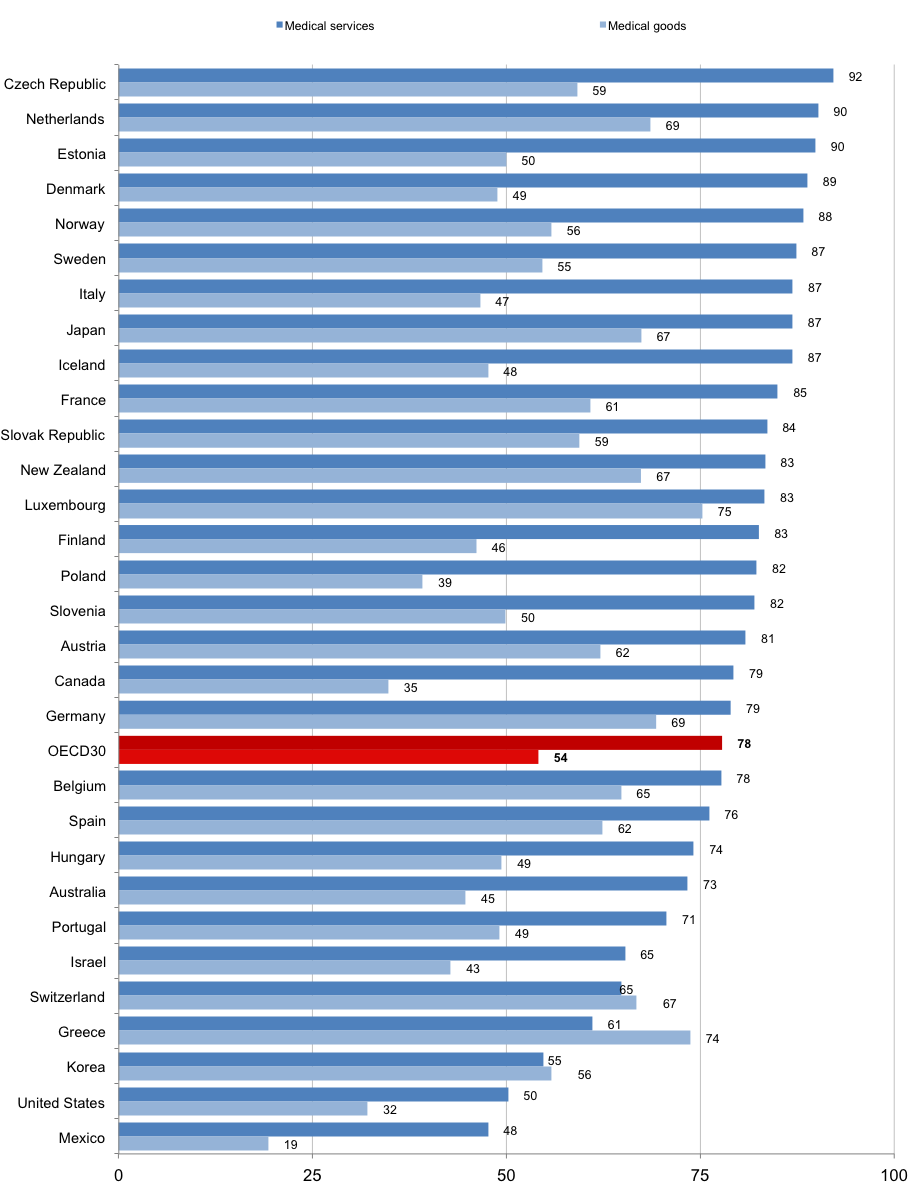
OECD: Public share of expenditure on medical services and goods, 2011 (or nearest year); Click image to zoom.
Hospital beds are a very rough proxy for how much capacity a system has. In 1980, the US had 4.4 hospital beds available for every 1,000 citizens. By 2000, that number had dropped to 3.5, and in 2010, it was down to 3.1 beds per 1,000. The average in all OECD countries is just under five.
There’s no economic incentive for a private company to maintain staff and equipment that might never be needed. It’s an example of how efficiency can come at a high price. “We’ve got to build some more fat into this system,” says O’Sullivan, “or we are going to get caught flat-footed.”
The other imperative is disease surveillance — the vitally important task of quickly determining a pattern of infection when scattered patients in various locales first start appearing in emergency rooms. This is a primary function of the Centers for Disease Control, which is working with a slightly smaller budget today than it had in 2008, despite population growth and inflation.
We can gain some insight into how our health care system might function during a major infectious disease outbreak. In 2000, the US ran a multi-agency “drill” known as TOPOFF. Local, state and federal agencies simulated the release of Yersinia pestis — the bacterium that causes the plague — in Denver, Colorado, and studied what would have occurred had it been the real thing.
On the very first day of the exercise, hospital capacity became overtaxed and understaffing in crucial areas of the system became apparent. Low drug stocks, poor communication and overwhelmed caregivers were all factors in a rapid deterioration of care.
By the third day of the simulation, the study’s authors noted: “Medical care is beginning to shut down in Denver.” Some time into the first week of the outbreak, as people reacted to travel restrictions and forced isolation, civil unrest broke out. Soon after, officials conducting the exercise determined that the disease would had spread beyond the Rocky Mountain State.
At the end of the drill, “stores were closed. Food supplies ran out because no trucks were being let into the state. Rioting began to occur.” When the exercise was terminated, between 950 and 2000 people were “dead,” and the disease remained uncontrolled.
We are better prepared today than we were when TOPOFF was conducted — the US created the Strategic National Stockpile of medical supplies and pharmaceuticals, and it has grown in capacity significantly since the 9/11 attacks, despite recent cuts in spending on disease surveillance and prevention.
Nonetheless, public health experts say that a serious infectious disease outbreak is a matter of “when,” not “if.” And our persistent belief in the market’s ability to keep us healthy not only results in us paying more for health care than any other country for inferior results, it also leaves us open to a potentially disastrous infectious disease problem.

This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.